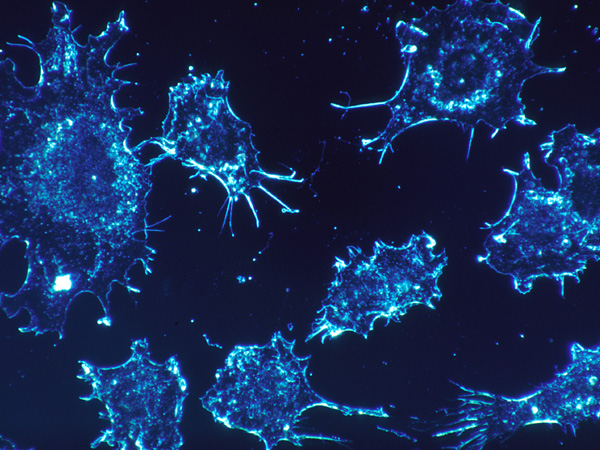
New York: Raising hopes for a cancer vaccine for different types of cancers, researchers have found that injecting minute amounts of two immune-stimulating agents directly into solid tumours in mice can eliminate all traces of cancer in the animals.
A clinical trial was launched in January to test the effect of the treatment in humans with lymphoma, cancer of the lymphatic system.
The approach works for many different types of cancers, including those that arise spontaneously, said the study published in the journal Science Translational Medicine.
The researchers believe the local application of very small amounts of the agents could serve as a rapid and relatively inexpensive cancer therapy that is unlikely to cause the adverse side effects often seen with bodywide immune stimulation.
“When we use these two agents together, we see the elimination of tumours all over the body,” said senior author of the study Ronald Levy, Professor at Stanford University School of Medicine in the US.
“This approach bypasses the need to identify tumour-specific immune targets and doesn’t require wholesale activation of the immune system or customisation of a patient’s immune cells,” Levy said.
“Our approach uses a one-time application of very small amounts of two agents to stimulate the immune cells only within the tumour itself. In the mice, we saw amazing, bodywide effects, including the elimination of tumours all over the animal,” Levy explained.
Cancers often exist in a strange kind of limbo with regard to the immune system. Immune cells like T cells recognise the abnormal proteins often present on cancer cells and infiltrate to attack the tumour. However, as the tumour grows, it often devises ways to suppress the activity of the T cells.
Levy’s method works to reactivate the cancer-specific T cells by injecting microgram (one-millionth of a gram) amounts of two agents directly into the tumour site.
One, a short stretch of DNA called a CpG oligonucleotide, works with other nearby immune cells to amplify the expression of an activating receptor called OX40 on the surface of the T cells.
The other, an antibody that binds to OX40, activates the T cells to lead the charge against the cancer cells.
Because the two agents are injected directly into the tumour, only T cells that have infiltrated it are activated. In effect, these T cells are “prescreened” by the body to recognise only cancer-specific proteins.
“This is a very targeted approach,” Levy said.
“Only the tumour that shares the protein targets displayed by the treated site is affected. We’re attacking specific targets without having to identify exactly what proteins the T cells are recognising,” Levy added.
—IANS