Washington D.C.: By examining the oral mycobiome, including all the fungi that might live there may lead to a possible treatment using fungi that may someday lead to better cavity prevention measures and treatments in children, says a new study.
Biological sciences assistant professor Vincent Richards led the study published in the journal of Applied and Environmental Microbiology.
“This work provides valuable insight into the oral mycobiome and the role fungi play in the mouth as it relates to caries,” said Richards. “If we understand that better then researchers can develop better cavity prevention measures. For example, perhaps they can put beneficial fungal species into a probiotic treatment.”
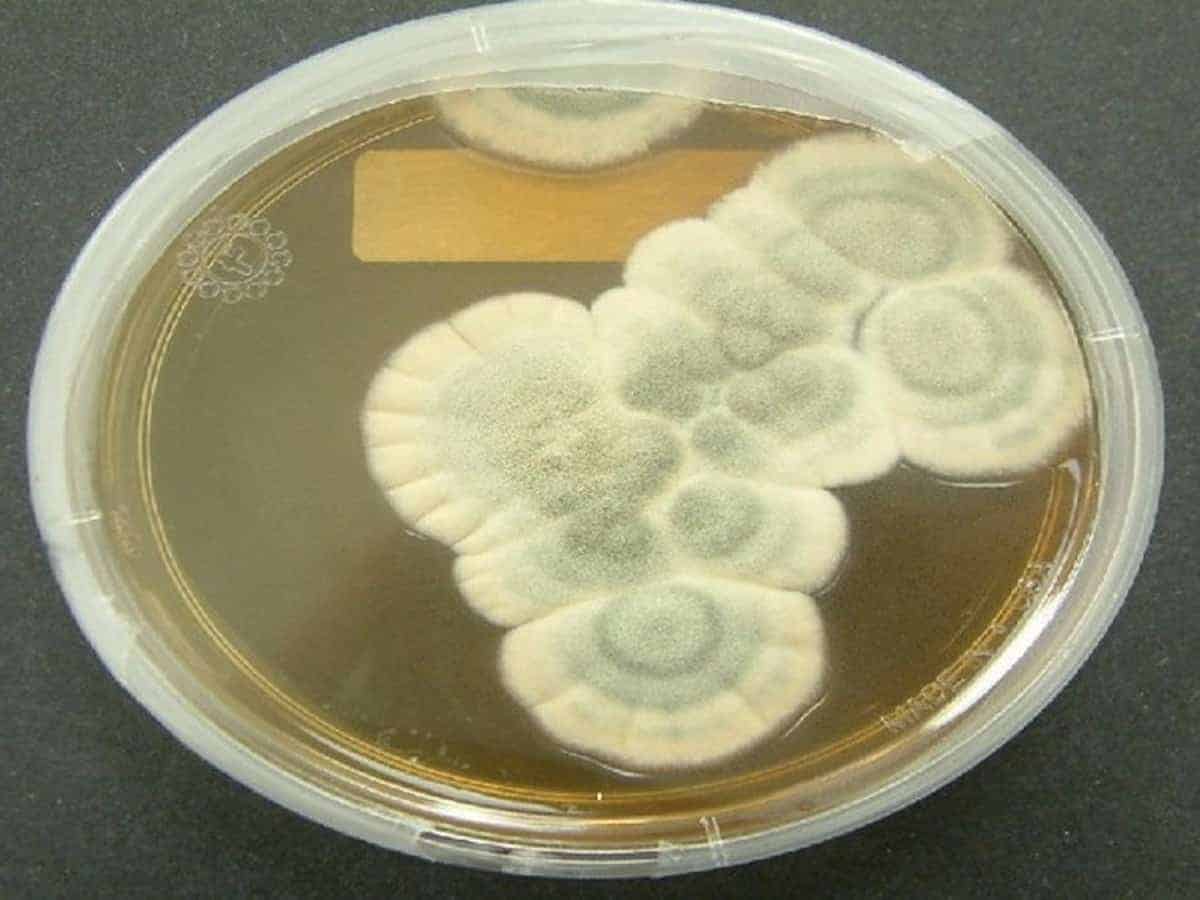
For years, the dental community has known that tooth decay occurs when the good and bad bacteria in our mouth become imbalanced and forms a biofilm (aka plaque). The biofilm absorbs the sugars we eat and the bacteria catabolize those sugars, turning them into acid, which decalcifies the teeth and causes cavities.
Thanks to advances in genome sequencing technology, scientists recently discovered that there is also a high diversity of fungi in the mouth, albeit in far fewer numbers than bacteria. However, little was known about the fungi’s role in cavity formation and caries disease progression.
“The microbiome is a community-based thing and it’s very complex,” said biological sciences graduate student Lauren O’Connell, the lead author of the study. “Because fungi are present in the tooth biofilm, they’re capable of utilizing these same sugars [as bacteria] and can produce acid, but we don’t fully understand their role.”
In the study, O’Connell sequenced the DNA from plaque samples of 33 children with varying stages of tooth health, including healthy teeth with no cavities; teeth with enamel lesions, which are indicative of an early-stage cavity; and teeth with dentin lesions, which indicate an advanced-stage cavity requiring either a filling or extraction.
She also examined the condition of the patients’ mouths, including a mouth with no cavities or lesions; a mouth with some teeth that have enamel lesions; and a mouth that has some teeth with enamel and dentin lesions.
“By looking at two variables–tooth and mouth health–we are taking a site-specific approach, which enables us to categorize each plaque sample six ways, or along a continuum,” said Richards. “This is important because we have found that the bacterial microbiome from a healthy tooth in a diseased mouth is more similar to the microbiome of a diseased tooth. That microbiome has shifted its profile to more of a diseased state.”
“We wanted to see how the microbiome community changed as the disease progressed,” explained O’Connell. “There’s only been one other study that looked at the fungi in relation to cavities, but they examined only healthy teeth and severely diseased teeth.”
The research team identified 139 species of fungus that live in human dental plaque, and of those, nine were strongly associated with dental health–in other words, they could be contributing to keeping teeth healthy.
The fungi associated with healthy teeth may be producing a compound called xylitol, which has been shown to inhibit the growth of the Streptococcus mutans bacteria that is known to cause cavities. Xylitol is an ingredient in sugarless gum.
“It’s possible that the nine fungi are promoting health by creating xylitol and other advanced microbial compounds,” said O’Connell. “But we have to do further functional testing to figure out if that is actually what is happening.”