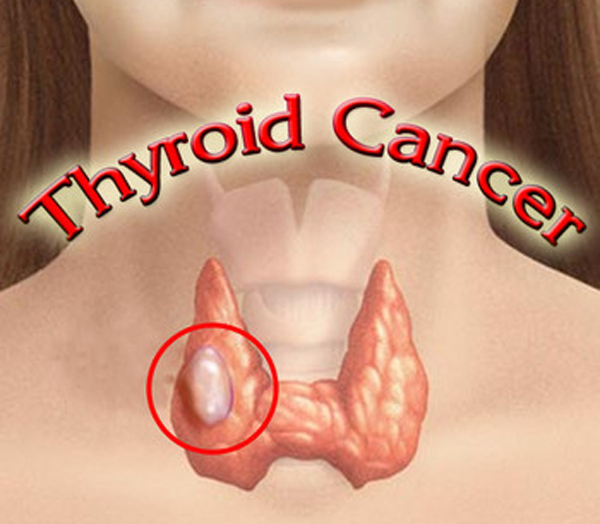
What is thyroid cancer?
Thyroid cancer is cancer that occurs in the butterfly-shaped thyroid gland located just below the Adam’s apple at the base of the neck, according to Mayo Clinic. The most common types of thyroid cancer, according to the American Cancer Society, include papillary carcinoma, follicular carcinoma and Hurthle cell carcinoma. Medullary thyroid carcinoma, anaplastic carcinoma, thyroid lymphoma and thyroid sarcoma are rare forms of the disease.

Thyroid cancer- Causes :
Thyroid cancer is linked with a number of inherited conditions (described in Thyroid cancer risk factors), but the exact cause of most thyroid cancers is not yet known.
Certain changes in a person’s DNA can cause thyroid cells to become cancerous. DNA is the chemical in each of our cells that makes up our genes – the instructions for how our cells function. We usually look like our parents because they are the source of our DNA. But DNA affects more than just how we look. It also can influence our risk for developing certain diseases, including some kinds of cancer.
Some genes contain instructions for controlling when our cells grow and divide into new cells. Certain genes that help cells grow and divide or make them live longer than they should are called oncogenes. Other genes that slow down cell division or make cells die at the right time are called tumor suppressor genes. Cancers can be caused by DNA changes that turn on oncogenes or turn off tumor suppressor genes.
People inherit 2 copies of each gene – one from each parent. We can inherit damaged DNA from one or both parents. Most cancers, though, are not caused by inherited gene changes. In these cases, the genes change during a person’s life. They may occur when a cell’s DNA is damaged by something in the environment, like radiation, or they may just be random events that sometimes happen inside a cell, without an outside cause.
Types of thyroid cancer:
The type of thyroid cancer you have determines treatment and prognosis. Types of thyroid cancer include:
• Papillary thyroid cancer. The most common form of thyroid cancer, papillary cancer arises from follicular cells, which produce and store thyroid hormones. Papillary thyroid cancer can occur at any age, but most often it affects people ages 30-50.
• Follicular thyroid cancer. Follicular cancer also arises from the follicular cells of the thyroid. It usually affects people older than age 50. Hurthle cell cancer is a rare and potentially more aggressive type of follicular thyroid cancer.
• Medullary thyroid cancer. Medullary thyroid cancer begins in thyroid cells called C cells that produce the hormone calcitonin. Elevated levels of calcitonin in the blood can detect medullary thyroid cancer at a very early stage. Certain genetic syndromes increase the risk of medullary thyroid cancer, although this genetic link is uncommon.
• Anaplastic thyroid cancer. Anaplastic thyroid cancer is a rare and rapidly growing cancer that is very difficult to treat. Anaplastic thyroid cancer typically occurs in adults age 60 or older.
• Thyroid lymphoma. Thyroid lymphoma is a rare form of thyroid cancer that begins in the immune system cells in the thyroid and grows very quickly. Thyroid lymphoma typically occurs in older adults.

Thyroid Cancer -Symptoms:
People with thyroid cancer often experience the following symptoms or signs. Sometimes, people with thyroid cancer do not show any of these symptoms. Or, these symptoms may be caused by a medical condition that is not cancer.
• A lump in the front of the neck, near the Adam’s apple
• Hoarseness
• Swollen glands in the neck
• Difficulty swallowing
• Difficulty breathing
• Pain in the throat or neck
• A cough that persists and is not caused by a cold
• Lump in the Neck: Not all thyroid nodules are big enough to cause a noticeable lump. Some people, though, may notice a lump in the front of their neck. You may be able to see it, or perhaps you can’t see it but you can feel it. Other people may notice a lump in your neck when you swallow. The most common way that a thyroid lump (and potential thyroid cancer) is detected, however, is when a doctor performs a thyroid exam and feels your thyroid.
• Swollen Lymph Node: Swollen lymph nodes in the neck are another symptom of thyroid cancer (a symptom not related to thyroid nodules). Thyroid cancer can spread to the lymph nodes, which are scattered throughout your body to help you fight infection. The lymph nodes in your neck (you can feel them under your jaw) become swollen when you have a cold or sore throat, for example. When the infection is gone, they should return to their normal size, so if the lymph nodes in your neck stay enlarged for an extended period—and you aren’t sick—you should talk to your doctor.
• Hoarse Voice: Your thyroid gland sits just below the larynx (more commonly known as your voice box). A thyroid nodule (which may be thyroid cancer) may be pressing on the voice box, causing hoarseness or voice changes. This is an uncommon way that thyroid cancer is detected.
• Difficulty Swallowing or Breathing: The thyroid is on top of your trachea—the windpipe. A developing thyroid cancer may put pressure on your trachea, making breathing more difficult. Your esophagus is below your trachea, so again, a developing thyroid cancer can cause trouble swallowing. This is also an uncommon way that thyroid cancer is detected.
• Neck Pain: Pain is usually a clue that something in your anatomy isn’t working quite as it should. If you have neck pain that lasts longer than a few weeks, you should make an appointment with your doctor to figure out what’s causing it. Thyroid cancer is a rare cause of neck pain but if you have neck pain combined with some of these other symptoms, be sure to mention that to your doctor.
• Throat Pain: Similar to neck pain, if you have throat pain that won’t go away, you should go to see your doctor. It’s a possible symptom of thyroid cancer.
The above symptoms are associated with thyroid nodules of all types, not just cancerous nodules. Since most thyroid cancers develop in thyroid nodules, it’s essential to be aware of these symptoms and signs that may point to thyroid cancer. Keep in mind, however, that the majority of thyroid nodules are not cancerous, and most adults will have a thyroid nodule (or even a few of them).
The symptoms of thyroid cancer are hard to detect—and usually the noticeable symptoms are caused not by the cancer itself but by the thyroid nodule where the thyroid cancer is developing. If you notice any of these signs or symptoms, make an appointment with your doctor.

Thyroid cancer- Diagnosis:
Doctors use many tests to diagnose cancer and find out if it has spread to another part of the body, called metastasis. Some tests may also determine which treatments may be the most effective. For most types of cancer, a biopsy is the only way to make a definitive diagnosis of cancer.
If a biopsy is not possible, the doctor may suggest other tests that will help make a diagnosis. Imaging tests may be used to find out whether the cancer has spread.
Your doctor may consider these factors when choosing a diagnostic test:
• Age and medical condition
• Type of cancer suspected
• Signs and symptoms
• Previous test results
The list below describes options for diagnosing this type of cancer. Not all tests listed will be used for every person.
• Physical examination: The doctor will feel the neck, thyroid, throat, and lymph nodes (the tiny, bean-shaped organs that help fight infection) in the neck for unusual growths or swelling. If surgery is recommended, the larynx may be examined at the same time with a laryngoscope, a thin, flexible tube with a light.
• Blood tests: There are several types of blood tests that may be done during diagnosis and to monitor the patient during and after treatment. This includes tests called tumor marker tests. Tumor markers are substances found at higher than normal levels in the blood, urine, or body tissues of some people with cancer.
• Thyroid hormone levels: As explained in the Overview, thyroid hormones regulate a person’s metabolism. The doctor will use this test to find out the current levels of the thyroid hormones triiodothyronine (T3) and thyroxine (T4) in the body.
• TSH: This blood test measures the level of thyroid-stimulating hormone (TSH), a hormone produced by the pituitary gland near the brain. If the body is in need of thyroid hormone, the pituitary gland releases TSH to stimulate production.
• Tg and TgAb: Thyroglobulin (Tg) is a protein made naturally by the thyroid. After treatment, there should be very low levels of thyroglobulin in the blood since the goal of treatment is to remove all thyroid cells. A tumor marker test may be done to measure the body’s Tg level before, during, and/or after treatment. There is also a test for thyroglobulin antibodies (TgAb), which are proteins produced by the body to attack thyroglobulin that occur in some patients. If TgAb is found, it is known to interfere with the results of the Tg level test.
• Medullary type-specific tests: If MTC is a possibility, the doctor will order tumor marker tests to check for high calcitonin and carcinoembryonic antigen (CEA) levels. The doctor may also recommend a blood test to detect the presence of RET proto-oncogenes (see Risk Factors), particularly if there is a family history of MTC.
• Ultrasound: An ultrasound uses sound waves to create a picture of the internal organs. An ultrasound wand or probe is guided over the skin of the neck area. High-frequency sound waves create a pattern of echoes that show the doctor the thyroid gland size and specific information about any nodules, including whether a nodule is solid or a fluid-filled sac called a cyst.
• Biopsy: A biopsy is the removal of a small amount of tissue for examination under a microscope. Other tests can suggest that cancer is present, but only a biopsy can make a definite diagnosis. The way to determine whether a nodule is malignant or benign is through a biopsy. During this procedure, the doctor removes cells from the nodule that are then examined by a cytopathologist. A cytopathologist is a doctor who specializes in analyzing cells and tissue to diagnose disease.
A biopsy for thyroid nodules will be done one of two ways:
• Fine needle aspiration: This procedure is usually performed in a doctor’s office or clinic. It is an important diagnostic step to determine if a thyroid nodule is benign or malignant. A local anesthetic may be injected into the skin to numb the area before the biopsy. The doctor inserts a thin needle into the nodule and removes cells and some fluid. The procedure may be repeated two or three times to obtain samples from different areas of the nodule. The report done by the pathologist. A pathologist is a doctor who specializes in interpreting laboratory tests and evaluating cells, tissues, and organs to diagnose disease. The test can be positive, meaning there are cancerous cells, or negative, meaning there are no cancerous cells. The test can also be undetermined, meaning it is not clear whether cancer is there.
• Surgical biopsy: If the needle aspiration biopsy is not clear, the doctor may suggest a biopsy in which the nodule and possibly the affected lobe of the thyroid will be removed. This procedure is usually done under general anesthesia; it may require a hospital stay.
• Molecular testing of the tumor: Your doctor may recommend running laboratory tests on a tumor sample to identify specific genes, proteins, and other factors unique to the tumor. Results of these tests will help decide whether your treatment options include a type of treatment called targeted therapy (see Treatment Options).
• Radionuclide scanning: This test may also be called a full-body scan or a radioactive iodine (also called I-131 or RAI) scan. It is used most often to learn more about a thyroid nodule. In this test, the patient swallows a very small, harmless amount of radioactive iodine, which is absorbed by thyroid cells. This makes the thyroid cells appear on the scan image, allowing the doctor to see differences between those cells and other body structures.
• X-ray: An x-ray is a way to create a picture of the structures inside of the body, using a small amount of radiation. For instance, a chest x-ray can help doctors determine if the cancer has spread to the lungs.
• Positron emission tomography (PET) scan: A PET scan is a way to create pictures of organs and tissues inside the body. A small amount of a radioactive sugar substance is injected into the patient’s body. This sugar substance is taken up by cells that use the most energy. Because cancer tends to use energy actively, it absorbs more of the radioactive substance. A scanner then detects this substance to produce images of the inside of the body.
After diagnostic tests are done, your doctor will review all of the results with you. If the diagnosis is thyroid cancer, these results also help the doctor describe the cancer; this is called staging.


Thyroid Cancer – Treatment:
This section outlines treatments that are the standard of care (the best known treatments available) for this specific type of cancer. When making treatment plan decisions, patients are also encouraged to consider clinical trials as an option.
A clinical trial is a research study to test a new approach to treatment to evaluate whether it is safe, effective, and possibly better than the standard treatment. Clinical trials may test such approaches as a new drug, a new combination of standard treatments, or new doses of current therapies. Your doctor can help you review all treatment options. For more information, see the About Clinical Trials and Latest Research sections.
Treatment overview:
In cancer care, different types of doctors often work together to create a patient’s overall treatment plan that combines different types of treatments. This is called a multidisciplinary team. Cancer care teams also include a variety of other health care professionals, including physician assistants, oncology nurses, social workers, pharmacists, counselors, dietitians, and others.
For thyroid cancer, this team may also include a surgeon, medical oncologist, radiation oncologist, and endocrinologist, which is a doctor specializing in problems with hormones, glands, and the endocrine system.
Thyroid cancer is commonly treated by one or a combination of treatments. Descriptions of these treatment options are listed below, followed by an outline of common cancer treatments given by stage of disease (see Stages).
Treatment options and recommendations depend on several factors, including:
• The type and stage of cancer
• Possible side effects
• The patient’s preferences
• The patient’s overall health
Take time to learn about your treatment options and be sure to ask questions about things that are unclear. Also, talk about the goals of each treatment with your doctor and what you can expect while receiving the treatment.
Cancer treatment is often selected based on guidelines recommended by panels of expert physicians. Although most thyroid cancer is curable, there can be different opinions in how to treat thyroid cancer, particularly regarding which combination of treatments to use and the timing when treatments are done. Patients are encouraged to seek a second opinion before starting treatment because they should be comfortable with the treatment plan they choose and should ask about clinical trials.
Surgery:
Surgery is the removal of the tumor and some surrounding healthy tissue during an operation. Surgery may also be called a resection. It is the main treatment for most people with thyroid cancer. A surgical oncologist is a doctor who specializes in treating cancer using surgery. Depending on the size of the nodule, common surgical options include:
• Lobectomy: This surgery removes the gland’s lobe with the cancerous nodule.
• Near-total thyroidectomy: Also called subtotal thyroidectomy, this is surgery to remove the thyroid gland except for a small part.
• Total thyroidectomy: This surgery removes the entire thyroid gland.
There are different surgical techniques that can be used for a thyroidectomy
• Conventional thyroidectomy: This is when the surgeon makes one large incision near the base or middle of the neck. This gives the surgeon direct access to the patient’s thyroid gland for the operation. At some cancer centers, newer surgical techniques are being offered to reduce or avoid neck scarring.
• An endoscopic thyroidectomy: During this procedure, the surgeon makes several small incisions and then inserts a video camera and surgical instruments to complete the surgery.
• Robotic thyroidectomy: The surgeon makes an incision elsewhere, such as in an armpit or chest, then uses a robotic tool to complete the surgery.
Not all surgical options are recommended for all patients. Talk with your doctor about the best approach to treat you.
If there is evidence or risk of spread of cancer to the lymph nodes in the neck, the surgeon may also perform a neck dissection. This is surgery to remove the lymph nodes in the neck that can also be called a lymphadenectomy.
In general, complications of thyroid surgery may include damage to the nearby parathyroid glands that help regulate blood calcium levels, excessive bleeding, or wound infections. If the nerves to the larynx are damaged during surgery, this may cause temporary or permanent hoarseness or a “breathy” voice.
Without the thyroid gland, the body stops producing thyroid hormone, which is essential to a body’s functioning. Hormone replacement (see below), usually given by a daily pill, is the best solution. The patient may also have to take vitamin D and calcium supplements if the parathyroid gland function is impaired after surgery.
If a tumor cannot be removed using surgery, it is called unresectable. The doctor will then recommend other treatment options.
Hormone treatment:
Patients who are treated with surgery for papillary, follicular, and medullary thyroid cancer require thyroid hormone therapy. In addition to replacing the hormone that is needed by the body, the thyroid hormone medication will slow down the growth of any remaining differentiated cancer cells.
Thyroid hormone replacement is levothyroxine (Levothroid, Levoxyl, Synthroid, Tirosint, Unithroid, and other brand names.) Levothyroxine typically comes as a pill that should be taken daily, at the same time each day, so that the body receives a consistent supply. Also, be sure to talk with your doctor about all other medications you take, including dietary supplements such as iron or calcium, to avoid interactions with your thyroid hormone replacement. Read more about tips to take your medication correctly.
Thyroid pills may have a few side effects. Occasionally, some patients develop a rash or lose some hair during the first months of treatment.
Hyperthyroidism, which is too much hormone, may cause weight loss, chest pain, rapid heart rate, irregular heartbeat, cramps, diarrhea, a feeling of being hot, sweats, and bone loss or osteoporosis.
Hypothyroidism, which is too little hormone, may cause fatigue, weight gain, dry skin and hair, and a feeling of being cold.
The amount or dose of thyroid hormone required is different for every patient and tumor type, and it can change as a person ages. The doctor will monitor your thyroid hormone levels through regular blood tests. Talk with your doctor about what signs to watch for that may mean it is time to adjust your dose, or amount, of hormone supplement.
Radioactive iodine (radioiodine) therapy:
The thyroid absorbs almost all iodine that enters a body. Therefore, a type of radiation therapy called radioactive iodine (also called I-131 or RAI) can find and destroy thyroid cells not removed by surgery and those that have spread beyond the thyroid. A doctor who specializes in giving radiation therapy to treat cancer is called a radiation oncologist.
This treatment is an option for most people with the papillary and follicular types. A small test dose may be given prior to full treatment to be sure the tumor cells will absorb the I-131. Patients with MTC or anaplastic thyroid cancer are not treated with I-131.
I-131 therapy is given in either liquid or pill form. Patients receiving I-131 to destroy cancer cells may or may not be hospitalized for two to three days, depending on several factors including the dose given. Patients are encouraged to drink fluids to help the I-131 pass quickly through the body.
Within a few days, most of the radiation is gone. Talk with your doctor about ways to limit radiation exposure to other people, including children, who may be around you during this treatment and the days following it.
In preparation for radioactive iodine treatment after surgery, patients are usually asked to follow a low-iodine diet for two to three weeks beforehand. In addition to the low-iodine diet, patients will be asked to either stop taking thyroid hormone replacement pills temporarily or receive injections of recombinant TSH (Thyrogen) while taking the hormone replacement. If the hormone therapy is stopped during the preparation period, the patient will likely experience side effects due to hypothyroidism (see above).
It is important to discuss the possible short-term and long-term effects of I-131 therapy with your doctor. On the first day of treatment, patients may experience nausea and vomiting. In certain circumstances, pain and swelling can occur in the areas where the radioactive iodine is collected.
Because iodine is concentrated in salivary gland tissue, patients may experience swelling of the salivary glands. This may result in xerostomia, sometimes called dry mouth.
Large or cumulative doses of radioactive iodine may cause infertility, which is the inability to produce a child, especially in men. It is recommended that women avoid pregnancy for at least one year after radioactive iodine treatment. There is a risk of secondary cancer with the use of I-131 (see the section on Follow-up Care). Occasionally, patients may require repeated radioactive treatments over time. However, there is a maximum total dose of radioactive iodine allowed over time, and once reached; this may prevent further use of this treatment.
External-beam radiation therapy:
External-beam radiation is another type of radiation therapy in which high-energy x-rays are given from a machine outside the body to destroy cancer cells. An external-beam radiation therapy regimen (schedule) usually consists of a specific number of treatments given oven a set period of time. When used to treat thyroid cancer, radiation therapy is usually given as outpatient therapy, either in a hospital or clinic, five days a week for about five to six weeks.
For thyroid cancer, external-beam radiation therapy is used only in certain circumstances, typically when later-stage thyroid cancer has not responded to I-131 radioactive iodine therapy (see above). Radiation therapy is usually given after surgery, and treatment is concentrated on a specific area, only affecting cancer cells at that site.
Side effects depend on the treatment dosage and area and may include redness of the skin, odynophagia (painful swallowing), cough, occasional hoarseness, nausea, and fatigue. Most side effects go away soon after treatment is finished.
Chemotherapy and Targeted therapy:
Chemotherapy is the use of drugs to destroy cancer cells and is sometimes used to treat thyroid cancer. Chemotherapy is given by a medical oncologist, a doctor who specializes in treating cancer with medication. A chemotherapy regimen (schedule) usually consists of a specific number of cycles given over a set period of time. A patient may receive one drug at a time or combinations of different drugs at the same time.
Systemic chemotherapy gets into the bloodstream to reach cancer cells throughout the body.
Common ways to give chemotherapy include an intravenous (IV) tube placed into a vein using a needle or in a pill or capsule that is swallowed. The goal of chemotherapy can be to destroy cancer remaining after surgery, slow the tumor’s growth, or reduce symptoms.
The side effects of chemotherapy depend on the individual and the dose used, but they can include: Fatigue, risk of infection, nausea and vomiting, hair loss, loss of appetite, and diarrhea. These side effects usually go away once treatment is finished.
Targeted therapy is a treatment that targets the cancer’s specific genes, proteins, or the tissue environment that contributes to cancer growth and survival. This type of treatment blocks the growth and spread of cancer cells while limiting damage to normal cells. Learn more about the basics of targeted therapy.
Recent studies show that not all tumors have the same targets. To find the most effective treatment, your doctor may run tests to identify the genes, proteins, and other factors in your tumor. This helps doctors better match each patient with the most effective treatment whenever possible. In addition, many research studies are taking place now to find out more about specific molecular targets in the different types of thyroid cancer and new treatments directed at them.
For papillary and follicular thyroid cancer, the U.S. Food and Drug Administration (FDA) has approved two targeted therapies:
• In 2013, the FDA approved a targeted therapy called sorafenib (Nexavar) for later-stage or recurrent differentiated thyroid cancer when I-131 therapy (see above) has not worked. Learn more in a 2013 summary here. Common side effects of sorafenib include hand-foot skin reactions or other skin problems, diarrhea, fatigue, weight loss, and high blood pressure.
• In February 2015, the FDA approved a targeted therapy called lenvatinib (Lenvima, E7080) for later-stage differentiated thyroid cancer that does not respond to surgery and/or I-131 treatment. The side effects of lenvatinib include high blood pressure, diarrhea, decreased appetite, decreased weight, and nausea. More details about this drug can be found in a 2014 study summary here.
For MTC, there are two other FDA-approved targeted therapy options:
• In 2011, the FDA approved vandetanib tablets (Caprelsa, zd6474), which is a type of targeted therapy known as a tyrosine kinase inhibitor. Specifically, vandetanib is now a standard treatment for adults when MTC is not able to be removed surgically, the disease is worsening, or if MTC has spread to other parts of the body.
The medication is given as a daily pill; the typical daily dose of vandetanib is 300 mg. Common side effects include diarrhea and colon inflammation, skin rash, nausea, high blood pressure, headache, fatigue, loss of appetite, and stomach pain. Additionally, more serious side effects such as respiratory and heart problems can occur. Blood tests, including serum potassium, calcium, magnesium, and TSH levels (see Diagnosis), may be done to monitor the body’s reaction to this medication on a regular basis.
• In 2012, the FDA approved another tyrosine kinase inhibitor for metastatic MTC called cabozantinib (Cometriq, XL184). The recommended dose is 140 mg, taken in pill form once daily. Side effects may include constipation, stomach pain, high blood pressure, hair color changes, fatigue, nausea, and swelling, in addition to serious colon problems.
Before any targeted treatment begins, talk with your doctor about possible side effects for each specific medication and how they can be managed.
At this time, the use of other, systemic chemotherapy and targeted therapy for the treatment of thyroid cancer is determined on an individual basis and is most often given as part of a clinical trial. See the Latest Research section for more information.
Learn more about the basics of chemotherapy and preparing for treatment. The medications used to treat cancer are continually being evaluated. Talking with your doctor is often the best way to learn about the medications prescribed for you, their purpose, and their potential side effects or interactions with other medications. Learn more about your prescriptions by using searchable drug databases.
Getting care for symptoms and side effects :
Cancer and its treatment often cause side effects. In addition to treatment to slow, stop, or eliminate the cancer, an important part of cancer care is relieving a person’s symptoms and side effects. This approach is called palliative or supportive care, and it includes supporting the patient with his or her physical, emotional, and social needs.
Palliative care is any treatment that focuses on reducing symptoms, improving quality of life, and supporting patients and their families. Any person, regardless of age or type and stage of cancer, may receive palliative care. It works best when palliative care is started as early as needed in the cancer treatment process.
People often receive treatment for the cancer and treatment to ease side effects at the same time. In fact, patients who receive both often have less severe symptoms, better quality of life, and report they are more satisfied with treatment.
Palliative treatments vary widely and often include medication, nutritional changes, relaxation techniques, emotional support, and other therapies. You may also receive palliative treatments similar to those meant to eliminate the cancer, such as chemotherapy, surgery, or radiation therapy. Talk with your doctor about the goals of each treatment in your treatment plan.
Before treatment begins, talk with your health care team about the possible side effects of your specific treatment plan and palliative care options. And during and after treatment, be sure to tell your doctor or another health care team member if you are experiencing a problem so it can be addressed as quickly as possible. Learn more about the basics of palliative care.
Treatment options by stage:
If the thyroid cancer is only within the tissues of the neck, both in the thyroid gland and in the lymph nodes, surgery will typically be the first treatment. Patients with later stage disease may be treated with surgery as well, but other treatments may be done first. Clinical trials may be recommended at any stage as a treatment option.
Stage I: Surgery; hormone therapy; possible radioactive iodine therapy after surgery
Stage II: Surgery; hormone therapy; possible radioactive iodine therapy after surgery
Stage III: Surgery; hormone therapy; possible radioactive iodine therapy or external-beam radiation therapy after surgery
Stage IV: Surgery, hormone therapy, radioactive iodine therapy, external-beam radiation therapy, targeted therapy, and chemotherapy. Radiation therapy may also be used to reduce pain and other problems.
Stage IV thyroid cancer:
If the cancer has spread beyond the thyroid to other organs, such as the bones or lungs, it is called metastatic or Stage IV thyroid cancer. Also, all anaplastic thyroid tumors are classified as stage IV at the time of diagnosis, regardless of tumor size, location, or spread.
Patients with this diagnosis are encouraged to talk with doctors who are experienced in treating this stage of cancer, because there can be different opinions about the best treatment plan. Learn more about getting a second opinion before starting treatment, so you are comfortable with the treatment plan chosen. This discussion may include clinical trials.
Your health care team may recommend a treatment plan that includes a combination of surgery, hormone therapy, radioactive iodine therapy, external-beam radiation therapy, targeted therapy, and chemotherapy. Clinical trials on new treatment approaches may also be recommended.
Palliative care will also be important to help relieve symptoms and side effects
For most patients, a diagnosis of metastatic cancer is very stressful and, at times, difficult to bear. Patients and their families are encouraged to talk about the way they are feeling with doctors, nurses, social workers, or other members of the health care team. It may also be helpful to talk with other patients, including through a support group.


Thyroid Cancer Prevention:
Preventing thyroid cancer is in many cases impossible, but certain steps may reduce the risk.
Exposure to X-rays is a proven cause of thyroid cancer, and young children may be most at risk. Therefore, it may be wise to minimize X-rays in children.
Although it is typically not a problem in the United States, people should consume a diet that contains iodine. Foods with iodine include fish, shellfish, eggs, dairy products, onions, radishes, potatoes, bananas, parsley, and kelp. In the United States, most table salt contains iodine.
If a family member had or has medullary thyroid cancer and is found to have the familial form of the disease, siblings, children and parents should be tested at an early age to see if they have inherited a gene that makes thyroid cancer more common. If they have the gene, they may opt to have the thyroid surgically removed to lessen the risk of cancer.