New York: In a fight against novel coronavirus, researchers have developed a human cell ‘membrane on a chip’ that allows continuous monitoring of how drugs and infectious agents interact with our cells.
It may soon be used to test potential drug candidates for Covid-19.
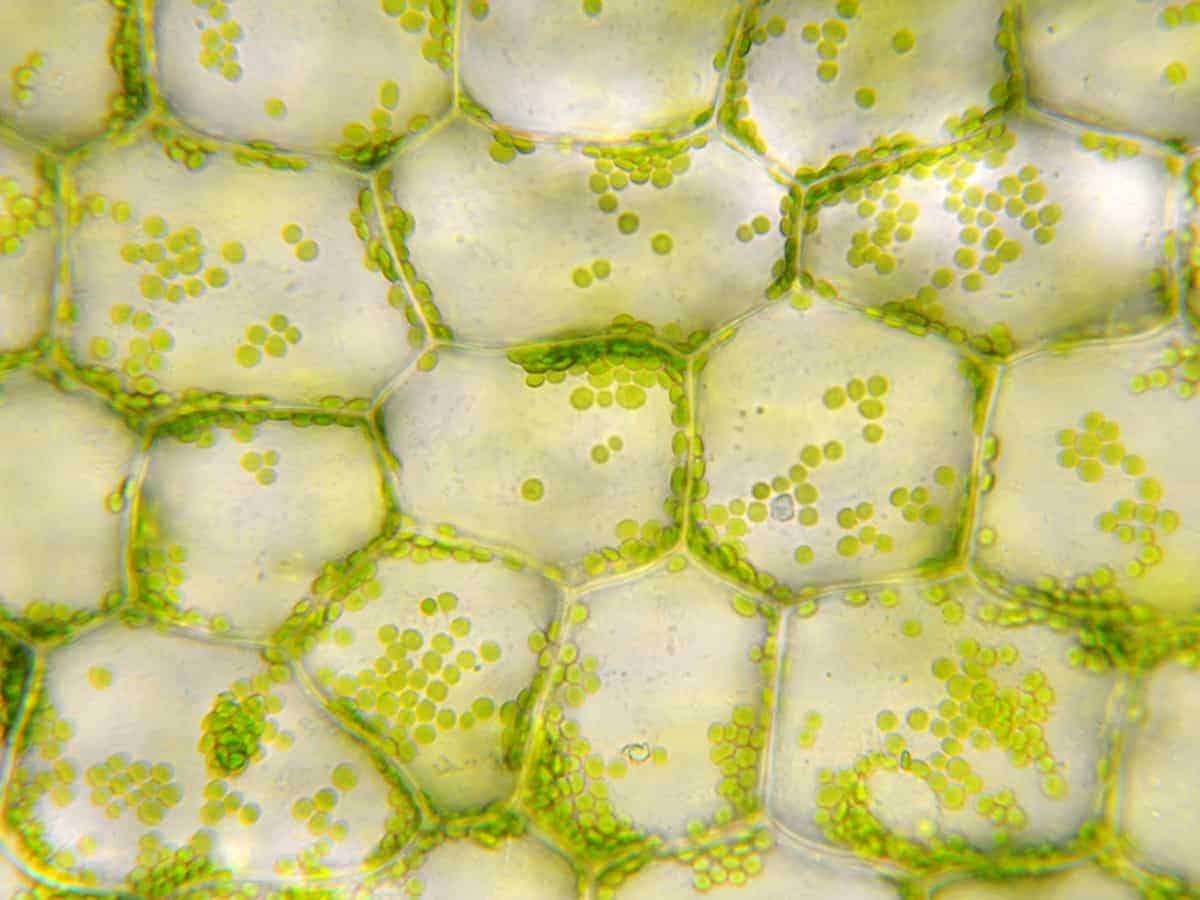
The study, published in the journals ACS Langmuir and ACS Nano, revealed that the device could mimic any cell type–bacterial, human or even the tough cells walls of plants.
According to the researchers from the University of Cambridge in the UK, Cornell University and Stanford University in the US, their research recently pivoted to how COVID-19 attacks human cell membranes and, more importantly, how it can be blocked.
They have been successfully used to monitor the activity of ion channels, a class of protein in human cells which are the target of more than 60 per cent of approved pharmaceuticals.
“This type of screening is typically done by the pharmaceutical industry with live cells, but our device provides an easier alternative,” said study researcher Dr R�is�n Owens from Cambridge’s Department of Chemical Engineering and Biotechnology.
“This method is compatible with high-throughput screening and would reduce the number of false positives making it through into the R&D pipeline,” Owens added.
According to the researchers, cell membranes play a central role in biological signalling, controlling everything from pain relief to infection by a virus, acting as the gatekeeper between a cell and the outside world.
The team set out to create a sensor that preserves all of the critical aspects of a cell membrane–structure, fluidity, and control over ion movement–without the time-consuming steps needed to keep a cell alive.
The device uses an electronic chip to measure any changes in an overlying membrane extracted from a cell, enabling the scientists to safely and easily understand how the cell interacts with the outside world.
The device integrates cell membranes with conducting polymer electrodes and transistors.
To generate the on-chip membranes, the Cornell team first optimised a process to produce membranes from live cells and then, working with the Cambridge team, coaxed them onto polymeric electrodes in a way that preserved all of their functionality.
The hydrated conducting polymers provide a more ‘natural’ environment for cell membranes and allow robust monitoring of membrane function.
The Stanford team optimised the polymeric electrodes for monitoring changes in the membranes.
The device no longer relies on live cells that are often technically challenging to keep alive and require significant attention, and measurements can last over an extended time period.
“Because the membranes are produced from human cells, it’s like having a biopsy of that cell’s surface – we have all the material that would be present including proteins and lipids, but none of the challenges of using live cells,” said study senior author Dr Susan Daniel from Cornell University.
“The device can be as small as the size of a human cell and easily fabricated in arrays, which allows us to perform multiple measurements at the same time,” said study researcher Anna-Maria Pappa from Cambridge University.