WashingtonD.C. [USA]: A recent study has identified RNA-based biomarkers that distinguish between normal, aging hematopoietic stem cells and leukemia stem cells associated with secondary acute myeloid leukemia (sAML), a particularly problematic disease that typically afflicts older patients who have often already experienced a bout with cancer.
The findings suggest a new way to predict leukemic relapse early and to identify potential targets for new drug development.
Secondary AML typically follows a chronic pre-malignant disease or treatment for other cancers. Consequently, patients tend to be diagnosed later in life, usually after the age of 60.
Senior author Catriona Jamieson said, “Because of relatively low survival rates and their advancing age, these patients tend to be poor candidates for aggressive therapies, like a bone marrow transplant,”
“There is a pressing need for more effective treatments that prevent disease progression and relapse,” she added.
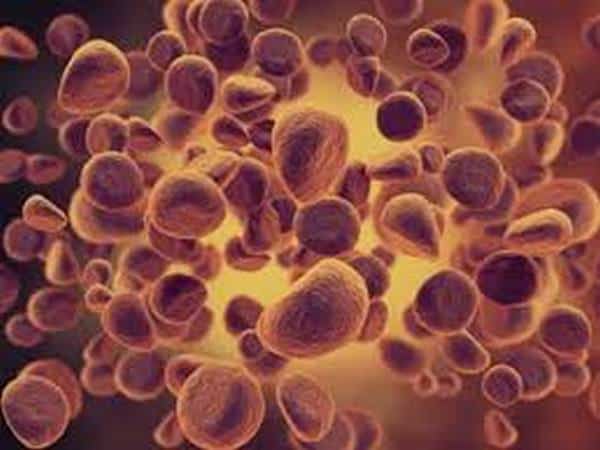
Aging is a key risk factor for sAML because, over time, hematopoietic stem cells (which give rise to all other blood cell types) accumulate DNA mutations and changes in other molecules that put DNA instructions into action, such as RNA and proteins.
Jamieson’s team wanted to understand how RNA might change with the aging of normal blood stem cells compared with sAML stem cells.
“By being able to distinguish benign from malignant aging based on distinctive RNA splicing patterns, we can develop therapeutic strategies that selectively target leukemia stem cells while sparing normal hematopoietic stem cells,” she said.
Leslie Crews, co-first author, said the team “specifically looked at a process called RNA splicing, which is responsible for removing pieces of extraneous RNA that do not contain instructions to make protein. If disrupted, RNA splicing could enhance the capacity of cells to propagate cancer.”
Using sensitive genetic sequencing technology, the scientists identified unique RNA splicing variants that distinguish normal, aging stem cells from abnormal, malignant ones.
“These splicing signatures could potentially be used as clinical biomarkers to detect blood stem cells that show signs of early aging or leukemia, and to monitor patient responses to treatment,” said Crews.
Current AML therapies fail to eliminate dormant leukemia stem cells responsible for disease relapse.
“Our findings show that RNA splicing is a unique therapeutic vulnerability for secondary AML,” said Jamieson, adding, “RNA-splicing-targeted therapies may be a potent and selective way to clear leukemia stem cells and prevent relapse.”
The researchers also tested a small molecule splicing modulator compound derived from a natural product and developed in the lab.
In patient-derived animal models, they found that just three doses of the compound, called 17S-FD-895, significantly reduced the ability of leukemia stem cells to self-renew. The authors say it’s the first study to show RNA splicing modulators inhibit cancer stem cell activity.
“While genetic and proteomic tools can address the mechanisms of splicing at a global level, small molecule modulators allow the selective examination of splicing mechanism,” said Burkart.
“This work was enabled by our ability to prepare stable analogs of natural products that modulate the spliceosome and represents more than 10 years of effort into synthetic and medicinal chemistry,” he added.
“We are optimistic that these findings will support our long term goal of delivering a clinical candidate to combat blood-borne cancer. Furthermore, we see these materials as important probes to dissect the complex yet important mechanics of disease related splicing events.
Crews noted that RNA splicing-targeted agents have been shown to have activity in a variety of solid tumors so the findings may be relevant to a variety of cancers, such as breast and drug-resistant melanoma.
The research was published online in Cell Stem Cell. (ANI)