Boston: A team of researchers, in an effort to improve the survival of patients with myeloproliferative neoplasms, a type of leukemia, inhibited a specific protein to decrease the number of large bone marrow cells in an experimental model.
An increase in megakaryocyte numbers is thought to be the cause of many problems observed in this disease. This type of treatment approach has never been attempted before.
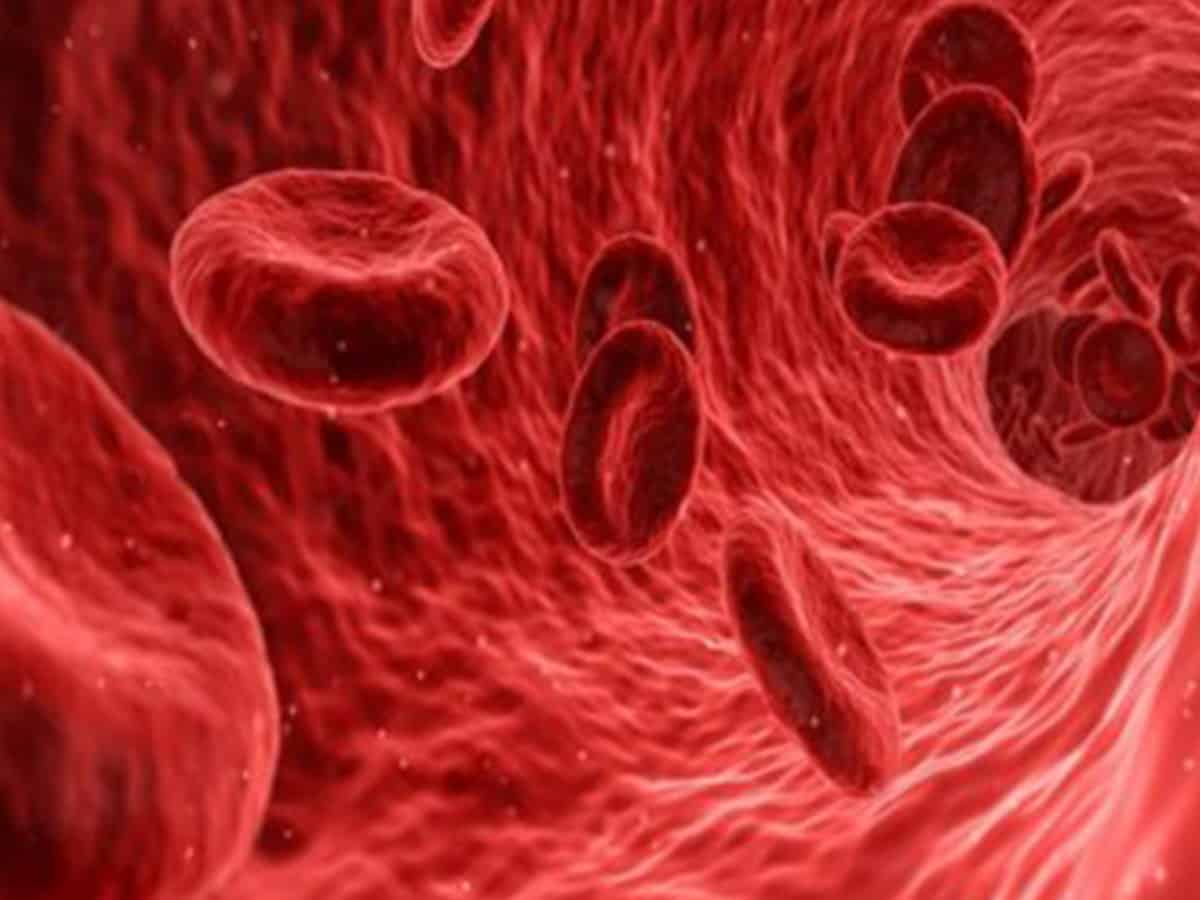
Myeloproliferative neoplasms are a type of blood cancer that begins with a pathological mutation (change) in a stem cell in the bone marrow which causes too many red blood cells, white blood cells, or platelets to be produced.
Most patients die of the transformation of the disease to a more fatal leukemia or because of myelofibrosis, scarring of bone marrow. There are currently no specific treatments for myelofibrosis.
“To date, most drug development efforts have been focused on the JAK2V617F mutation, but this approach has failed to fundamentally change the course of the disease. Our study has taken a totally new approach for the treatment of the disease, which, if successful, will present a complementary or even an alternative therapy to existing treatments,” explained lead author Shinobu Matsuura, DVM, PhD, instructor of medicine at Boston University School of Medicine (BUSM).
Using two sets of experimental models, the researchers altered the JAK2V617F gene in one group to induce symptoms of myeloproliferative neoplasms.
The second group were the control. When both groups were exposed to an antibody against alpha5beta1 integrin, the number of megakaryocytes decreased in bone marrow in the group with the altered gene, while no changes were seen in the control group.
According to the researchers, their ultimate objective is to find effective treatments for myelofibrosis, which can occur secondary to many diseases and is a terminal condition with no specific treatment available.
“Myeloproliferative neoplasms are a chronic and debilitating disease. Safe and effective novel treatments of this disease will improve the quality of life of these patients,” the researchers said.
These findings appear online in the journal Blood.