Pneumonia :
Pneumonia is an infection of the lungs that is caused by bacteria, viruses, fungi, or parasites. It is characterized primarily by inflammation of the alveoli in the lungs or by alveoli that are filled with fluid (alveoli are microscopic sacs in the lungs that absorb oxygen).
At times a very serious condition, pneumonia can make a person very sick or even cause death. Although the disease can occur in young and healthy people, it is most dangerous for older adults, babies, and people with other diseases or impaired immune systems.
In the United States, more than 3 million people develop pneumonia each year, and about 17% of these receive treatment in a hospital. Most people with pneumonia recover, but about 5% will succumb to the condition.

Causes of Pneumonia:
Many germs can cause pneumonia. Examples include different kinds of bacteria, viruses, and, less often, fungi.
Most of the time, the body filters germs out of the air that we breathe to protect the lungs from infection. Your immune system, the shape of your nose and throat, your ability to cough, and fine, hair-like structures called cilia (SIL-e-ah) help stop the germs from reaching your lungs. (For more information, go to the Diseases and Conditions Index How the Lungs Work article.)
Sometimes, though, germs manage to enter the lungs and cause infections. This is more likely to occur if:
Your immune system is weak
A germ is very strong
Your body fails to filter germs out of the air that you breathe
For example, if you can’t cough because you’ve had a stroke or are sedated, germs may remain in your airways. (“Sedated” means you’re given medicine to make you sleepy.)
When germs reach your lungs, your immune system goes into action. It sends many kinds of cells to attack the germs. These cells cause the alveoli (air sacs) to become red and inflamed and to fill up with fluid and pus. This causes the symptoms of pneumonia.
Germs That Can Cause Pneumonia:
Bacteria: Bacteria are the most common cause of pneumonia in adults. Some people, especially the elderly and those who are disabled, may get bacterial pneumonia after having the flu or even a common cold.
Many types of bacteria can cause pneumonia. Bacterial pneumonia can occur on its own or develop after you’ve had a cold or the flu. This type of pneumonia often affects one lobe, or area, of a lung. When this happens, the condition is called lobar pneumonia
The most common cause of pneumonia in the United States is the bacterium
Streptococcus (strep-to-KOK-us) pneumoniae, orpneumococcus (nu-mo-KOK-us).
Lobar Pneumonia: Another type of bacterial pneumonia is called atypical pneumonia. Atypical pneumonia includes:
Legionella pneumophila: This type of pneumonia sometimes is called Legionnaire’s disease, and it has caused serious outbreaks. Outbreaks have been linked to exposure to cooling towers, whirlpool spas, and decorative fountains.
Mycoplasma pneumonia: This is a common type of pneumonia that usually affects people younger than 40 years old. People who live or work in crowded places like schools, homeless shelters, and prisons are at higher risk for this type of pneumonia. It’s usually mild and responds well to treatment with antibiotics. However, mycoplasma pneumonia can be very serious. It may be associated with a skin rash and hemolysis (the breakdown of red blood cells).
Chlamydophila pneumonia: This type of pneumonia can occur all year and often is mild. The infection is most common in people 65 to 79 years old.

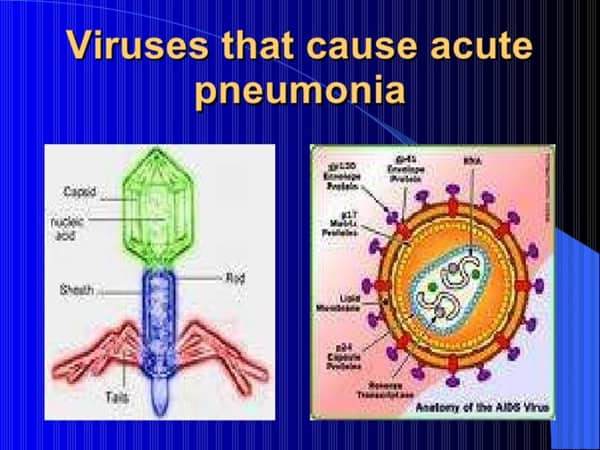
Viruses:
Respiratory viruses cause up to one-third of the pneumonia cases in the United States each year. These viruses are the most common cause of pneumonia in children younger than 5 years old.
Most cases of viral pneumonia are mild. They get better in about 1 to 3 weeks without treatment. Some cases are more serious and may require treatment in a hospital.
If you have viral pneumonia, you run the risk of getting bacterial pneumonia as well.
The flu virus is the most common cause of viral pneumonia in adults. Other viruses that cause pneumonia include respiratory syncytial virus, rhinovirus, herpes simplex virus, severe acute respiratory syndrome (SARS), and more.
Fungi:
Three types of fungi in the soil in some parts of the United States can cause pneumonia. These fungi are:
Coccidioidomycosis (kok-sid-e-OY-do-mi-KO-sis):- This fungus is found in Southern California and the desert Southwest.
Histoplasmosis (HIS-to-plaz-MO-sis):- This fungus is found in the Ohio and Mississippi River Valleys.
Cryptococcus (krip-to-KOK-us):- This fungus is found throughout the United States in bird droppings and soil contaminated with bird droppings.
Most people exposed to these fungi don’t get sick, but some do and require treatment.
Serious fungal infections are most common in people who have weak immune systems due to the long-term use of medicines to suppress their immune systems or having HIV/AIDS.
Pneumocystis jiroveci (nu-mo-SIS-tis ye-RO-VECH-e):- formerly Pneumocystis carinii, sometimes is considered a fungal pneumonia. However, it’s not treated with the usual antifungal medicines. This type of infection is most common in people who:
Have HIV/AIDS or cancer
Have had an organ transplant and/or blood and marrow stem cell transplant
Take medicines that affect their immune systems.

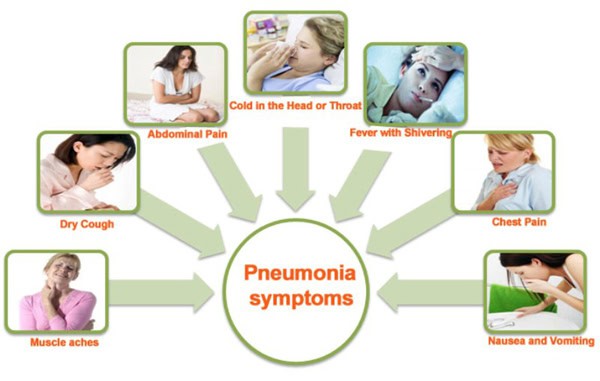
Symptoms :-
Pneumonia is a lung infection that can make you very sick. You
may cough, run a fever, and have a hard time breathing. For most people, pneumonia can be treated at home. It often clears up in 2 to 3 weeks. But older adults, babies, and people with other diseases can become very ill. They may need to be in the hospital.
You can get pneumonia in your daily life, such as at school or work. This is called community-associated pneumonia. You can also get it when you are in a hospital or nursing home. This is called healthcare-associated pneumonia. It may be more severe because you already are ill. This topic focuses on pneumonia you get in your daily life.
Germs called bacteria or viruses usually cause pneumonia.
Pneumonia usually starts when you breathe the germs into your lungs. You may be more likely to get the disease after having a cold or the flu. These illnesses make it hard for your lungs to fight infection, so it is easier to get pneumonia. Having a long-term, or chronic, disease likeasthma, heart disease, cancer, or diabetes also makes you more likely to get pneumonia.
Symptoms of pneumonia caused by bacteria usually come on quickly. They may include:
Cough. You will likely cough up mucus (sputum) from your lungs. Mucus may be rusty or green or tinged with blood.
Fever.
Fast breathing and feeling short of breath.
Shaking and “teeth-chattering” chills.
Chest pain that often feels worse when you cough or breathe in.
Fast heartbeat.
Feeling very tired or very weak.
Nausea and vomiting.
Diarrhea.
When you have mild symptoms, your doctor may call this “walking pneumonia.”
Older adults may have different, fewer, or milder symptoms. They may not have a fever. Or they may have a cough but not bring up mucus. The main sign of pneumonia in older adults may be a change in how well they think. Confusion or delirium is common. Or, if they already have alung disease, that disease may get worse.
Symptoms caused by viruses are the same as those caused by bacteria. But they may come on slowly and often are not as obvious or as bad.
How Is Pneumonia Spread?
The germs that cause pneumonia are usually found in the mouth and nose of the infected person. They can be spread easily to another person, either through the air or by touching a contaminated surface. Typically, they enter the person’s body through their mouth, nose, or eyes. When this happens, a battle begins — the person’s immune system tries to kill the germs, while the germs try to multiply.
Although a person with either viral or bacterial pneumonia is contagious, that person’s germs are more likely to cause an upper respiratory infection in another person (such as the common cold) than pneumonia. This is because many of the viruses and bacteria that cause people to get pneumonia are the same ones that cause upper respiratory infections.

Diagnosis :-
Chest X-ray showing pneumonia:-Your doctor will start by asking about your medical history and doing a physical exam, including listening to your lungs with stethoscope to check for abnormal bubbling or crackling sounds that suggest pneumonia.
If pneumonia is suspected, your doctor may recommend the following tests:
Blood tests: Blood tests are used to confirm an infection and to try to identify the type of organism causing the infection. However, precise identification isn’t always possible.
Chest X-ray: This helps your doctor diagnose pneumonia and determine the extent and location of the infection. However, it can’t tell your doctor what kind of germ is causing the pneumonia.
Pulse oximetry: This measures the oxygen level in your blood. Pneumonia can prevent your lungs from moving enough oxygen into your bloodstream.
Sputum test: A sample of fluid from your lungs (sputum) is taken after a deep cough and analyzed to help pinpoint the cause of the infection.
Your doctor might order additional tests if you’re older than age 65, are in the hospital, or have serious symptoms or health conditions. These may include:
CT scan: If your pneumonia isn’t clearing as quickly as expected, your doctor may recommend a chest CT scan to obtain a more detailed image of your lungs.
Pleural fluid culture: A fluid sample is taken by putting a needle between your ribs from the pleural area and analyzed to help determine the type of infection.

Treatment:
Treatment for pneumonia involves curing the infection and preventing complications. People who have community-acquired pneumonia usually can be treated at home with medication. Although most symptoms ease in a few days or weeks, the feeling of tiredness can persist for a month or more.
Specific treatments depend on the type and severity of your pneumonia, your age and your overall health. The options include:
Antibiotics: These medicines are used to treat bacterial pneumonia. It may take time to identify the type of bacteria causing your pneumonia and to choose the best antibiotic to treat it. If your symptoms don’t improve, your doctor may recommend a different antibiotics.

Cough medicine: This medicine may be used to calm your cough so that you can rest. Because coughing helps loosen and move fluid from your lungs, it’s a good idea not to eliminate your cough completely. In addition, you should know that very few studies have looked at whether over-the-counter cough medicines lessen coughing caused by pneumonia. If you want to try a cough suppressant, use the lowest dose that helps you rest.

Fever reducers/pain relievers: You may take these as needed for fever and discomfort. These include drugs such as aspirin, ibuprofen (Advil, Motrin IB, others) and acetaminophen (Tylenol, others).
Hospitalization:-
You may need to be hospitalized if:
You are older than age 65
You are confused about time, people or places
Your kidney function has declined
Your systolic blood pressure is below 90 millimeters of mercury (mm Hg) or your diastolic blood pressure is 60 mm Hg or above
Your breathing is rapid (30 breaths or more a minute)
You need breathing assistance
Your temperature is below normal
Your heart rate is below 50 or above 100
You may be admitted to the intensive care unit if you need to be placed on a breathing machine (ventilator) or if your symptoms are severe.
Children may be hospitalized if:
They are younger than age 2 months
They are lethargic or excessively sleepy
They have trouble breathing
They have low blood oxygen levels
They appear dehydrated

Preventions:-
Germs are all around us. But don’t panic, most of them are completely harmless. Some even do us good, like the bacteria in our gut that aid digestion. The important thing is to protect our families from the germs that can cause bacterial diseases and other infections.
if a person has a viral illness like the flu, tiny droplets of moisture from their mouth can carry germs into the air when they cough ,sneeze or even just breathe. These can contaminate any surface that they land on, or infect other people by being breathed in.
This is what we call the chain of infection – harmful bacteria and other germs being accidentally being passed from one person to the next and causing infection. Thankfully, the chain can be broken.
Breaking the chain of infection:-
The best way to stop the spread of germs is through good hygiene. Here are some ways to help:
Wash your hands regularly – especially before eating, before and after preparing food, and after coughing, sneezing or using the toilet or changing a nappy. In case water is not readily available, use Dettol Wipes to disinfect and clean your hands.

Cover your nose and mouth with a tissue when you cough or sneeze. Put any used tissues straight in the bin and wash your hands.
Handle and prepare food safely. Clean your hands and surfaces regularly, separate raw and cooked foods, cook food thoroughly and chill fresh & cooked foods to slow the growth of bacteria.
Vaccinations (or immunisations) are a great way to protect from serious infection. Make sure your family is up to date with their vaccinations recommended by your health care professional
Clean and disinfect surfaces regularly – especially food contact surfaces and regularly touched surfaces such as taps, door handles and telephone keypads
Clean or disinfect :-
Cleaning means removing dirt and some germs, usually with a detergent and a thorough rinse with hot running water. For many small items (such as cutlery and crockery), this is enough to make them safe to use.
Disinfecting means and killing most of the germs present. This is important for larger or fixed surfaces where thorough rinsing isn’t possible (such as work tops, toilets, sinks and telephone handsets). Regularly disinfecting the surfaces of your home is one of the best ways to prevent the spread of harmful germs and bacteria.
Remember, even in a clean home harmful bacteria can still find their way in. Explore our site for further information on common illnesses and our advice if you or your loved ones get poorly.