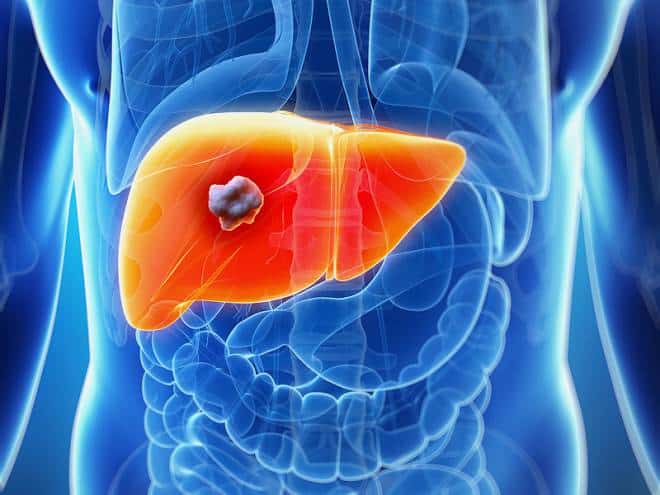
What is liver cancer?
Liver cancer consists of malignant hepatic tumors (growths) in or on the liver.
The most common type of liver cancer is hepatocellular carcinoma (or hepatoma, or HCC), and it tends to affect males more than females. According to the National Health Service (NHS), UK, approximately 1,500 people in the United Kingdom die from HCC each year.
The World Health Organization (WHO) estimate that liver cancer’s prevalence is around 30 cases per 100,000 people worldwide, with rates in parts of Africa and Eastern Asia being particularly high.

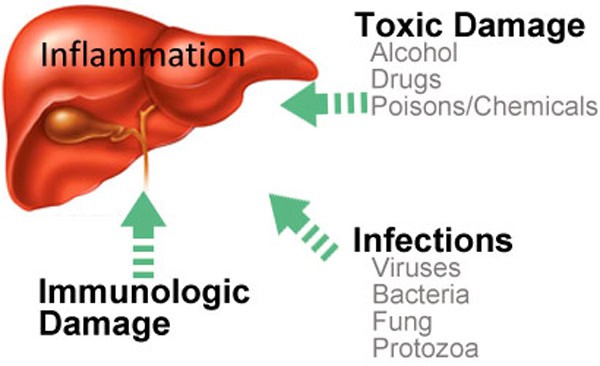
Causes of liver cancer:
Experts say that common causes of HCC are regular high alcohol consumption, having unprotected sex and injecting drugs with shared needles.
Anabolic steroids : Used by athletes and weight lifters. These male hormones, if used regularly and for long enough, can raise the risk of developing liver cancer, as well as some other cancers.
Aflatoxins : A substance made by a fungus and may be found in moldy wheat, groundnuts, corn, nuts, soybeans and peanuts. For liver cancer risk to increase there needs to be long-term exposure. This is more of a problem in less wealthy countries.
Cirrhosis : When liver cells are damaged and replaced with scar tissue. People with cirrhosis of the liver have a higher risk of developing liver cancer.
Diabetes : Patients with diabetes, especially if they also have hepatitis, or regularly consume a lot of alcohol, are more likely to develop liver cancer.
Family history : People whose mother, father, brother, or sister had liver cancer are at a higher risk of developing it themselves, compared to others.
L-carnitine deficiency : Studies suggest that an L-carnitine deficiency increases the risk of developing liver cancer.
Liver disease and inherited liver disease : People with hepatitis B or C have a significantly higher risk of developing liver cancer, compared to other healthy individuals. According to the American Cancer Society, hepatitis C is the most common cause of liver cancer in the USA. The Society mentions that some inherited liver diseases also increase the risk of liver cancer.
Low immunity : People with weakened immune systems, such as those with HIV/AIDS have a risk of liver cancer that is five times greater than other healthy individuals.
Obesity :Obesity raises the risk of developing many cancers, including liver cancer.
Gender : A higher percentage of males get liver cancer compared to females. Some experts believe this is not due to gender, but to lifestyle characteristics. On average, males tend to smoke and abuse alcohol more than females.
Smoking :Individuals with hepatitis B or C have a higher risk of liver cancer if they smoke.
Water wells with arsenic : People who rely on water wells that contain arsenic may eventually have a significantly higher risk of developing several conditions or diseases, including liver cancer.
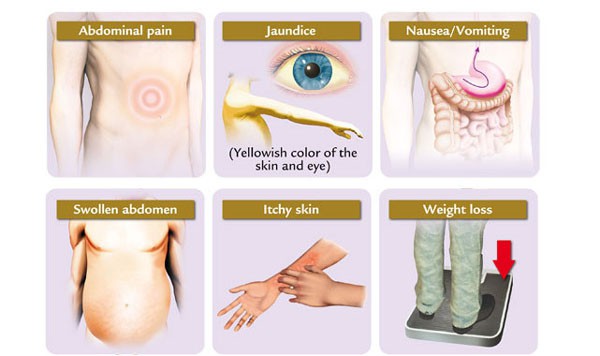
Symptoms of liver cancer
Signs and symptoms of liver cancer tend not to be felt or noticed until the cancer is well advanced.
Symptoms may include:
Jaundice – skin, tongue and whites of the eyes become yellow
Abdominal pain – often on the right side, may reach as high up as the shoulder
Unexplained weight loss
Hepatomegaly – enlarged liver, the abdomen may appear swollen
Fatigue
Nausea
Emesis (vomiting)
Back pain
General itching
Fever.
Is Cancer Contagious?
Cancer is NOT contagious: A healthy person cannot “catch” cancer from someone who has it. There is no evidence that close contact or things like sex, kissing, touching, sharing meals, or breathing the same air can spread cancer from one person to another.
Cancer cells from one person are generally unable to live in the body of another healthy person. A healthy person’s immune system recognizes foreign cells and destroys them, including cancer cells from another person.
Cancer transfer during organ transplant: There have been some cases in which organ transplants from people with cancer have been able to cause cancer in the person who got the organ. But there’s a major factor that makes this possible – people who get organ transplants take medicines that weaken their immune systems. This must be done so their immune system won’t attack and destroy the transplanted organ. This seems to be the main reason that cancer in a transplanted organ can, in rare cases, give cancer to the person who gets the organ. Organ donors are carefully screened to reduce this risk.
Cancer risk after transplant already high: Still, recent studies have shown that cancer is more common in people who get solid-organ transplants than in people who don’t – even when the donor doesn’t have cancer. This also appears to be due to the drugs that are given to reduce the risk of transplant rejection. Research has shown that the longer and more intensely the immune system is suppressed after transplant, the higher the risk of cancer. The drugs that allow the body to accept the organ also make the immune system less able to recognize and attack pre-cancer cells and the viruses that can cause cancer.
Cancer transfer during pregnancy: Even if a woman has cancer during pregnancy, the cancer rarely affects the fetus directly. Some cancers can spread from the mother to the placenta (the organ that connects the mother to the fetus), but most cancers cannot affect the fetus itself. In a few very rare cases, melanoma (a form of skin cancer) has been found to spread to the placenta and the fetus.
Germs are contagious: We know that germs (especially bacteria and viruses) can be passed from person to person through sex, kissing, touching, and sharing or preparing food. Some can even be spread by breathing the same air. But germs are much more likely to be a threat to a person with cancer than to a healthy person. This is because people with cancer often have weakened immune systems, especially when they’re getting treatment. They may not be able to fight off infections very well.
Liver Cancer Diagnostic Tests:
If you have symptoms of liver cancer, the first step is a physical exam. The doctor will:
Feel your abdomen to examine the liver, spleen and nearby organs
Check your abdomen for ascites, an abnormal accumulation of fluid
Examine your skin and eyes for signs of jaundice
If the doctor suspects liver cancer, you may have one or more of the following tests to diagnose it and find out if it has spread.
Blood tests: One common blood test detects alpha-fetoprotein (AFP), which can be a sign of liver cancer. Other blood tests may measure how well the liver is working.
Imaging tests, which may include:
CT or CAT (computed axial tomography) scans: This is usually the most reliable test for evaluating the extent of liver cancer. Our technology includes the precise triple-phase CT scan.
Ultrasound
Angiogram: The doctor injects dye into an artery. This allows the blood vessels in the liver to be seen on an X-ray.
Biopsy: A sample of tissue from the tumor or the healthy part of the liver is removed and looked at under a microscope. Healthy tissue may be tested to see how well the liver is working. A biopsy may be obtained by:
Fine needle aspiration (FNA): A thin needle is inserted into the liver to remove a small amount of tissue.
Core biopsy: This is similar to FNA, but a thicker needle is used to remove small cylinder-shaped samples (cores).
Laparoscopy: A small incision (cut) is made in the abdomen, and a thin, lighted tube (laparoscope) is inserted to view the tumor.
Surgical biopsy: Tissue is removed during an operation.
Treatments:
These treatments are generally recommended when the tumor has been found at an early stage. Many doctors will not use these treatments if the tumor is larger than 5 cm. These treatments are surgery, thermal ablation, percutaneous ethanol injection, and radiation therapy.
Surgery.
Surgery is the removal of the tumor and some surrounding healthy tissue during an operation. It is likely to be the most successful disease-directed treatment, particularly for patients with a tumor smaller than 5 cm. If the tumor has spread outside the liver, or if the patient has other serious illnesses, surgery may not be an option. A surgical oncologist is a doctor who specializes in treating cancer using surgery. Learn more about the basics of cancer surgery.
Two types of surgery are used to treat HCC:
Hepatectomy. When a portion of the liver is removed, the surgery is called a hepatectomy. A hepatectomy can be done only if the cancer is in one part of the liver and the liver is working well. The remaining section of liver takes over the functions of the entire liver. The liver may grow back to its normal size within a few weeks. A hepatectomy may not be possible if the patient has advanced cirrhosis, even if the tumor is small.
The side effects of a hepatectomy may include pain, weakness, fatigue, and temporary liver failure. The health care team will watch for signs of bleeding, infection, liver failure, or other problems that need immediate treatment.
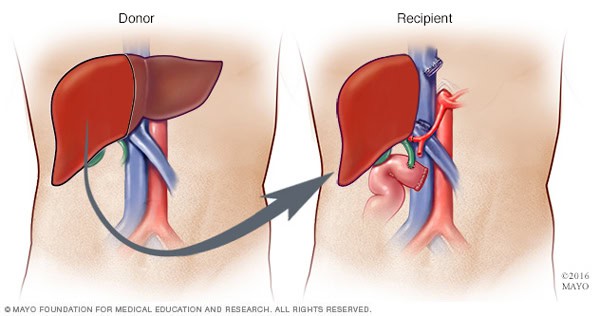
Liver transplantation. Sometimes, a liver transplantation can be done. This procedure is possible only when the cancer has not spread outside the liver, a suitable donor is found, and very specific criteria are met in terms of tumor size and number. These criteria usually are a single tumor 5 cm or smaller or 3 or fewer tumors, all of which are smaller than 3 cm. It is important to understand that the number of donor livers available is very limited, so transplantation is not always an option.
After a transplant, the patient will be watched closely for signs that the body might be rejecting the new liver or that the tumor has come back. The patient must take medication to prevent rejection. These drugs can cause side effects, such as puffiness in the face, high blood pressure, or increased body hair.
Liver transplantation is a particularly effective treatment for people with a small tumor because transplantation removes the tumor and the damaged liver. However, there are few donors, and people waiting for a liver transplant may have to wait for a long time before a liver becomes available. During this time, the disease may get worse. The transplant center will advise you on how long the wait is likely to be and what rules are used to prioritize people on the waiting list.
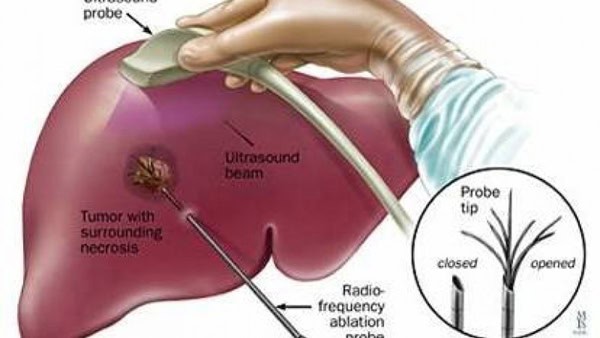
Thermal ablation.
Radiofrequency ablation (RFA) and microwave therapy both use heat to destroy cancer cells. They may be given through the skin, through laparoscopy, or during a surgical operation while a patient is sedated. Sedation is giving medication to become more relaxed, calm, or sleepy.
Percutaneous ethanol injection.
Percutaneous ethanol injection is when alcohol is injected directly into the liver tumor to destroy it. Side effects include fever and pain after the procedure. In general, the procedure is simple, safe, and particularly effective for a tumor smaller than 3 cm. However, if the alcohol escapes from the liver, a person may have brief but severe pain. This option is currently being used less often and has been largely replaced by RFA (see above).
Radiation therapy:
Radiation therapy is the use of high-energy x-rays or other particles to destroy cancer cells. A doctor who specializes in giving radiation therapy to treat cancer is called a radiation oncologist.
Stereotactic body radiation therapy (SBRT). SBRT is a term that describes several methods of delivering high doses of radiation to a tumor while limiting the amount of radiation to which healthy tissues are exposed. This is important because healthy liver tissue can be damaged by radiation. SBRT effectively treats tumors that are approximately 5 cm or smaller. However, it is still considered investigational compared to thermal ablation (see above) because little long-term information about its effectiveness exists.
Radioembolization is similar to chemoembolization (see below), except that during radioembolization, a doctor places radioactive beads into the artery that supplies the tumor with blood. The beads deliver radiation directly into the tumor when they become trapped in the small blood vessels of the tumor.
Side effects may include damage to the stomach and lungs. However, these side effects can often be prevented. Learn more about the basics of radiation therapy.
Disease-directed treatments to improve survival
If the doctor feels the cancer cannot be eliminated (cured) using 1 of the treatments listed above, he or she may recommend 1 of the following options to shrink the tumor and/or slow tumor growth. While these treatments will most likely not eliminate the cancer, they have been shown to improve duration of survival (length of life).
Chemoembolization:
This is a type of chemotherapy treatment that is similar to hepatic arterial infusion (see below). Chemotherapy is the use of drugs to destroy cancer cells. During this procedure, drugs are injected into the hepatic artery, and the flow of blood through the artery is blocked for a short time so the chemotherapy stays in the tumor longer. Blocking the blood supply to the tumor also destroys cancer cells.
In addition to being used as a primary treatment for HCC, chemoembolization may be used to slow tumor growth for people who are on the waiting list for liver transplantation.
Targeted therapy:
Targeted therapy is a treatment that targets the cancer’s specific genes, proteins, or the tissue environment that contributes to cancer growth and survival. This type of treatment blocks the growth and spread of cancer cells while limiting damage to healthy cells.
Recent studies show that not all tumors have the same targets. To find the most effective treatment, your doctor may run tests to identify the genes, proteins, and other factors in your tumor. This helps doctors better match each patient with the most effective treatment whenever possible. In addition, many research studies are taking place now to find out more about specific molecular targets and new treatments directed at them. Learn more about the basics of targeted treatments.
For HCC, anti-angiogenesis drugs are the most common targeted therapy. Anti-angiogenesis therapy is focused on stopping angiogenesis, which is the process of making new blood vessels. Because a tumor needs the nutrients delivered by blood vessels to grow and spread, the goal of anti-angiogenesis therapies is to “starve” the tumor. This is one of the ways sorafenib (Nexavar) is thought to work. Sorafenib is one of the treatment options for advanced HCC that cannot be completely removed with surgery. It is taken as pill that is swallowed (orally). The side effects of sorafenib include diarrhea and certain skin problems. Talk with your doctor about the possible side effects for a specific medication and how they can be managed.
Prevention:
Cancer prevention is action taken to lower the chance of getting cancer. By preventing cancer, the number of new cases of cancer in a group or population is lowered. Hopefully, this will lower the number of deaths caused by cancer.
To prevent new cancers from starting, scientists look at risk factors andprotective factors. Anything that increases your chance of developing cancer is called a cancer risk factor; anything that decreases your chance of developing cancer is called a cancer protective factor.
Some risk factors for cancer can be avoided, but many cannot. For example, both smoking and inheriting certain genes are risk factors for some types of cancer, but only smoking can be avoided. Regular exercise and a healthy diet may be protective factors for some types of cancer. Avoiding risk factors and increasing protective factors may lower your risk, but it does not mean that you will not get cancer.
Different ways to prevent cancer are being studied, including:
Changing lifestyle or eating habits.
Avoiding things known to cause cancer.
Taking medicines to treat a precancerous condition or to keep cancer from starting.