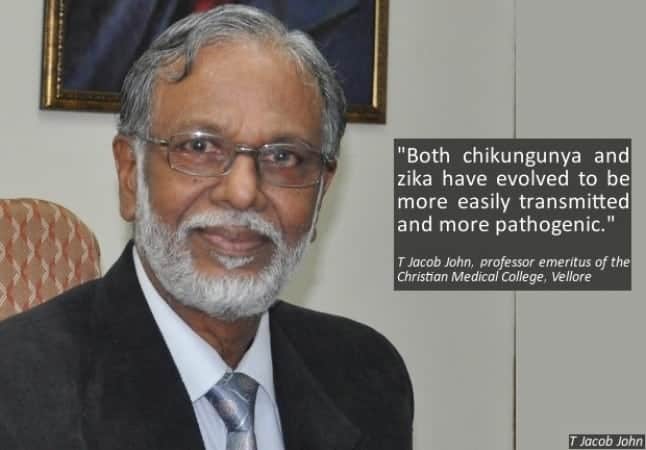
In an email interview, renowned virologist Dr T Jacob John, formerly with the Christian Medical College, Vellore, slammed the Indian and state governments for not testing enough for COVID-19.
He also warned that an “avalanche” of cases await the country. Here are excerpts from an email interview with the expert.
1. The original peak of the COVID-19 spread was expected to be around April 07-10. The lockdown was expected to flatten the curve to an extent and allow healthcare facilities to be prepared. Do you believe that south India (at least) is over the peak? Can we expect to see positive cases coming down?
Dr John: There is no mathematical modelling (for peak calculation); the inputs for such modelling are just not available. No state has reached the peak. How will we know if any state has reached the peak? (It is an) Old children’s story.
What did the bear see when it reached the top of the mountain? The other side of the mountain.
When the curve takes a downturn and stays the down-slope, then we know the peak was passed. We are yet to reach the peak. Things are going to get a lot worse as we all are moving towards the peak.
There is something called epidemiological intelligence and qualitative prediction arising out of all available information. Peak is several weeks away. Picture for India is grim. This is an avalanche.
2. How do you think the Tablighi Jamaat cluster has changed the curve for south Indian states? Some bureaucrats feel the peak has been pushed by two weeks, since they have not been able to carry out the requisite testing of all those who exhibit symptoms.
Dr John: There are several ways to see things. Because they were identifiable, they could be traced. India continued to behave as is life was absolutely normal even on March 22, when Parliament was sitting. On March 12, I wanted Health Emergency declared in India.
Instead, the Epidemic Act of 1897 was invoked. The red flagging of countries was slow and not strictly based on risk alone. Authentic information was not being given out on a daily basis like in New York or Kerala.
On March 21 we were given a very optimistic picture that staying indoors for 14 hours was sufficient. On March 24, out of the blue, came the 21-day lockdown. That is when people took things seriously.
Meanwhile southern States had been taking their own decisions – both good (for local battles) and bad (for national discipline as Epidemic detection and control is Union Government subject) during a national war.
Even now a lot of people are thinking that virus transmission will disappear by 18 days into lockdown. This morning, wearing a mask and keeping a safe – 6 feet – distance from others I went to buy milk to stock for the next several days.
The street was alive. I walked past a vegetable vendor. Three sellers – no mask. Seven buyers – only two with mask. All seven jostling to pick up vegetables.
My milk-booth vendor with no mask. I counted 100 people on the street and 39 had no mask.
Was there any “emergency”? Was there any mandate to wear masks? I suspect that the governments of the Union and Delhi were not guided properly by technical people.
So the Tablighi Jamaat became both victims and perpetrators. They were hit with double whammy. Universal mask use should have been mandated by mid-March.
3. Andhra Pradesh’s health secretary is the only one who has said there is some community spread in the state. Tamil Nadu and other south Indian states have maintained there is no community spread. What are your views? Is community transmission likely to have already taken place?
Dr John: What is definition of “community spread”? A traveller bringing infection is “travel-risk”. A contact getting infected is “contact infection”. If a contact of contact is infected, it is the very first link in the chain of community spread.
If an infected person has no identifiable contact with travel-risk or her/his contact, then it is community acquired. That has been going on from the time virus was introduced in all other states than Kerala. In India, community spread started by early March.
To say that was not happening is to go by “evidence” of community transmission. If you want such evidence you must apply a scientific method of looking. You don’t look and you don’t find and that was evidence that community spread was not occurring.
The error was compounded when the absence of evidence was taken as evidence of absence.
A person diagnosed infected today, signals an event that took place around two weeks ago. (It is like a ) star we see today was (actually) what it looked like light-years ago. Stray cases of “community-acquired” infection was known for weeks.
If you want evidence of community transmission before you take action to intercept it, that is a mistake. Your interception intervention must be blocking (proactive) and not pulling back (reactive). That needs epidemiological projection. Medical doctors are not familiar with that concept, because they have been taught to treat patients with evidence-based medicine.
In all these, Administrators – Health Secretaries for example – are developing biomedical/epidemiological information, instead of Directors of Health Services, NCDC Director etc.
If government does not trust them, perhaps governments are right, the technical leadership has not instilled confidence in administrators. (This is) Bad for a war on a virus.
4. Are we testing enough? If not, how much more testing should we be doing? (south Indian states and India as a whole too).
Dr John: What is enough? That is an epidemiological question for “public health” testing, the purpose of which is to find the source of transmission, quarantine, and protect the uninfected. For that the net is not thrown wide enough. So, answer is – not enough.
But once community spread has started and lockdown is declared, the importance of public health testing has reduced and need for “healthcare” testing has grown.
Healthcare testing is for the benefit of the infected, for his health. And for doctors to know their clinical diagnosis has been confirmed and the case is really COVID-19.
When test has to be rationed, as in India, the judgment is tactical (or strategic) for how much of public health testing and someone professional (statistical expert) ought to decide.
If a country is stingy on tests, then the test results cannot be used to determine epidemiology, speed or geography of spread. Test results can be used only to know the minimum number positive.
If 6000 are detected with “rationed” testing, then the true number could be 10 times or 20 times higher.
We need IgM testing for diagnosis of COVID-19 and IgG testing to certify who all are immune and can safely get back to normal economic activities. If we begin, we will be the first in the world. That is my own innovative idea to begin re-building economy.